If you work as a first responder, I’d like to start by saying thank you. Secondly, if you are one of the millions of first responders battling addiction, I want to tell you, there is hope.
We all owe a great debt of gratitude to our local emergency medical technicians, firefighters and police officers. You show up for your community in big ways, most notably in your willingness to enter situations full of unknowns with the confidence and competence needed to save lives.
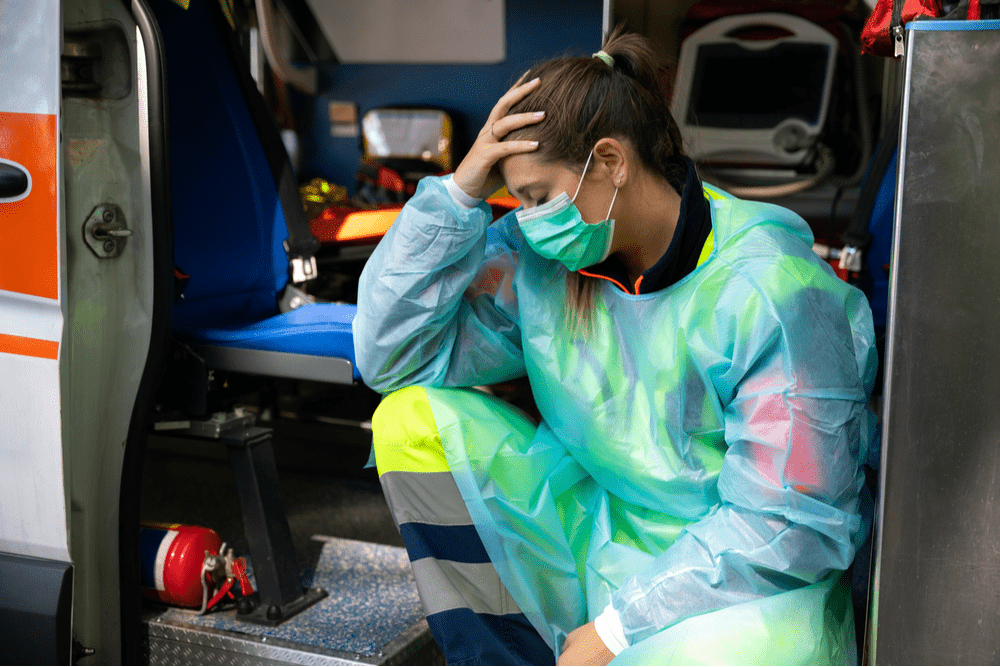
There’s no doubt you’ve seen some things. You’ve experienced some troubles. You’ve been through some trauma. And I bet that’s putting it mildly.
It’s no wonder, really, that you’ve found yourself looking for ways to cope.
As a small token of our appreciation for all that you do—and in an attempt to understand your unique suffering—today we’d like to offer up this word of encouragement:
You, our first responders, are human. It’s understandable to feel pain and hurt. You are expected to make mistakes. And you have the potential, just like anyone else, to right your wrongs and begin anew.
In fact, we’d love to help. Here at The Right Step Houston, we have a program specifically designed for you.
But first, let’s take a few minutes to discuss what research shows us about the nature of your job and the common ground you have among your peers, other first responders struggling with addiction. Then, we’ll get to the good part: hope.
The Life of a First Responder in Numbers
If you’re an EMT, firefighter or police officer, what we’re going to say next probably won’t surprise you. You’ve likely lived it. Still, we’d encourage you to read on because there’s a big difference between anecdotal evidence—what you observe around you—and facts derived from research.
Today we’re going to talk facts.
(And if you’re a friend or family member of a first responder, pay careful attention. You may be tempted to think your loved one is the odd-man or -woman out when, in reality, the risk factors for substance use disorder among our first responders is high.)
First responders often work grueling schedules and encounter all kinds of stressful situations. Social drinking and substance misuse as a coping mechanism result in EMTs, firefighters and police officers struggling with addiction at rates higher than the general population.
Studies show that more than half of firefighters report binge drinking in the past month. And around 17% of police officers drink at a level that interferes with their personal or professional life.
Maybe you’ve noticed a fellow coworker show up high or heard one call in sick because of a late night drinking or partying. Maybe you’ve done it yourself. You wouldn’t be alone. One survey found that two out of every three firefighters witnessed someone in their department come to work with a hangover. Two out of three!
There must be a reason our most-valued community servants—our first responders—struggle the way that they do. But before we get into the why, take a moment to check in with yourself and ask, “How do I feel about the assertion that there has to be a reason?”
After all, maybe you carry with you a great deal of shame because of your own actions. Or perhaps you find yourself judging the one you love—holding them to a higher standard because of their chosen profession.
Try, if you can, to set your preconceived notions aside. Extend grace to your friend or family member. Give a little grace to yourself. And read on . . .
A First Responder’s Job Comes With Legitimate Stressors and Risk Factors for Substance Use Disorder
Our first responders often show up to work with no idea what they’ll be asked to do that day and sometimes go home with a heavy heart and an aching body.
After all, firefighters risk severe burns and lung damage, police officers must be ready to face a suspect yielding a weapon, and EMTs meet people in their greatest moments of distress.
This, in addition to long hours, erratic work schedules, societal pressures and quota demands.
First Responders and Traumatic Events
Surveys show that a whopping 90% of our first responders have experienced trauma. And we can venture to guess that the remaining 10% will encounter something troubling soon enough.
Two other factors compound these findings:
- Many first responders keep these encounters to themselves. One study found that among police officers who had endured a distressing event less than half actually talked to someone at their agency about it.
- Nearly 70% of our first responders say they do not have enough time to recover between one traumatic event and the next.
So we have numerous firefighters, EMTs and police officers who not only endure trauma but do so repeatedly without communicating their needs or taking time to heal.
It’s no wonder, then, that 30% of first responders go on to develop behavioral health conditions like depression and PTSD (compared with just 20% of average American adults). Of course, these numbers leave many undiagnosed mental health disorders on the table—and many first responders reluctantly self-medicating their own despair.
Recognizing PTSD in Yourself or a Fellow First Responder
When stress is accepted as part of the job—a badge of honor even—it might be difficult to determine when your mental health could use some help. Maybe you do your job to the best of your ability and numb the pain as needed so you can . . . do your job to the best of your ability. But maybe you’re actually experiencing PTSD.
A few standard symptoms to be on the lookout for:
- Surprising outbursts of anger
- Inability to fall asleep
- Increasing anxiety or thoughts of depression
- A wandering mind that continually introduces flashbacks of traumatic moments
The Substance Abuse and Mental Health Services Administration offers a few off-the-beaten-path symptoms of PTSD as well:
- Watching TV for four hours or more each day
- Obsession over particular worries or concerns
- A complete refusal to think about or discuss prior traumatic events
If these ring true for you or a fellow first responder, and you also find yourself drinking more or using l drugs, it could be that you’re simply trying to cope with PTSD.
We want to remind you: you’re human. You weren’t meant to endure all the things you’ve been made to endure. It’s understandable that you would reach for a substance to help you manage what you’re feeling. But we want to help you find a better way. Interested? Keep reading, friend!
A Caveat About On-The-Job Injuries
Perhaps you’ve endured the same stressors mentioned above but found yourself struggling with addiction after following a different path altogether. After all, emotional pain is not the only one inflicted upon first responders.
Many traumatic events include on-the-job injuries, which lead to prescription pain medication and, sometimes, a reliance on opioids to continue functioning in a physically demanding job. That’s why painkillers have replaced alcohol as the substance most abused by police officers.
First Responders Battling Addiction: Dealing With Shame
In your role as a firefighter, EMT or police officer, you may feel especially discouraged by your substance misuse. After all, you likely entered this field to help others in your community and serve as a role model to the next generation.
Still, as we discussed, you’re human. I love the way David Givot, a former paramedic turned lawyer, now a first-responder advocate puts it: “[This] is a superhero’s business made up of flawed, mortal human beings who face the same demons as the rest of society.”
And that’s so true. You deserve the pedestal you are often placed upon, and yet, you’re human, just like the rest of us. And sometimes, we humans really mess up.
Maybe you drink too much. Or you use illegal drugs. Maybe you’ve even stolen pills from a patient during an opportune moment. And I’ll bet the thought really gets you down.
It’s important, though, that you work to reframe your shame into something more productive. After all, as Brene Brown says, “Shame corrodes the very part of us that believes we are capable of change.” In other words, if you simply sit in your shame, you may doubt that there’s a better way forward.
So what should you aim for instead? How about admitting guilt. Explains Brene:
“Shame is ‘I am bad.’ Guilt is ‘I did something bad.’ . . . Shame is highly correlated with addiction, depression . . . Guilt inversely correlated with all those things. The ability to hold something we’ve done or failed to do up against who we want to be is incredibly adaptive . . . it’s uncomfortable, but it’s adaptive.’”
In shame, we are stuck. In simply admitting guilt—even if only to ourselves at first—we have the opportunity to move forward.
Why Reaching Out for Help Is Worth Your Every Effort
The work you do is invaluable—and your community needs you to be at your very best. And you need that for yourself too.
You might be worried about what will happen if you admit your struggles and reach out for help, but of course, you probably also recognize what could happen if you don’t. Your job—and the life of someone in need—could one day hang in the balance.
And you can take heart when considering the scope of our society at large and the way addiction is often handled in first responders today. You can bet your agency is well aware of the stressors you face on a daily basis.
The U.S. Department of Justice states that it is the responsibility of law enforcement agencies to support their officers through counseling, trauma teams and education about substance abuse.
Police departments in San Diego, Los Angeles and Baltimore all created peer support groups in the past 10 years to help other first responders struggling with addiction—with up to one-third of employed officers during that time.
Getting help means you can get your life back—and get back to doing the work you love and that your community so desperately needs.
The Right Step Houston has a program specifically designed to help our first responders shake addiction for good—and learn to cope with the unique stressors you face every day. Give us a call at 844.768.0169 to learn more.
By Stephanie Thomas
Contributing Writer with Promises Behavioral Health